Inflammatory Bowel Disease: Crohn’s and Ulcerative Colitis
Crohn’s Disease and Ulcerative Colitis are the two main forms of Inflammatory Bowel Disease (IBD), affecting more than 300,000 people in the UK.
What are the symptoms?
- Diarrhoea – this is sometimes mixed with blood, mucus and pus
- Cramping pains in the abdomen – these can be very severe and often occur before passing a stool
- Tiredness and fatigue – this can be due to the illness itself, from anaemia (see below) from the side effects of some of the drugs used for IBD or from a lack of sleep if you have to keep getting up at night with pain or diarrhoea
- Feeling generally unwell – some people may feel feverish
- Loss of appetite and loss of weight – weight loss can be due to the body not absorbing nutrients from the food you eat because of the inflammation in the gut
- Anaemia (a reduced number of red blood cells) – you are more likely to develop anaemia if you are losing a lot of blood or not eating much
- Mouth ulcers
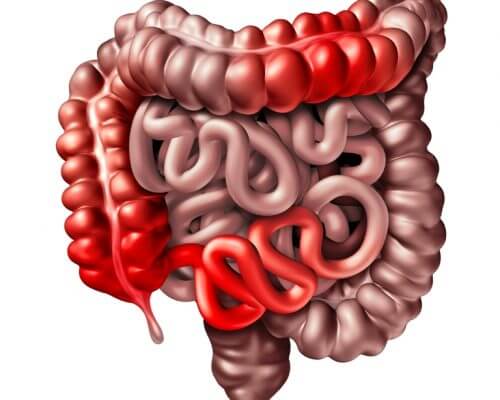
Some people with IBD, particularly Crohn’s, may develop complications, including:
- Strictures – this is when there is ongoing inflammation and the healing in the bowel may cause scar tissue to form. This can create a narrow section of the bowel, called a stricture
- Fistulas – a fistula is an abnormal channel or passageway connecting one internal organ to another, or to the outside surface of the body. These are more common in people with Crohn’s Disease. Read more about fistulas by clicking here
IBD can sometimes affect other parts of the body, including:
- Joints – inflammation of the joints, often known as arthritis, means that fluid collects in the joint space causing painful swelling. It usually affects the large joints of the arms and legs, including the elbows, wrists, knees and ankles
- Eye inflammation -– the most common eye condition affecting people with IBD is episcleritis, affecting the layer of tissue covering the white outer coating of the eye, making it red, sore and inflamed
Treatment for Crohn’s Disease and Ulcerative Colitis depends on how severe the symptoms are and how much of the gut is affected.
There are number of drugs used to treat IBD. In some cases, if medical treatment is not effective, then surgery may be required. Extensive resections (removal of diseased sections of the intestine) are now less common. However, surgery remains an important treatment option, often in combination with medical therapies.
- Strictureplasty – this is a way to treat strictures and blockages in the small intestine without having to remove any gut. The surgeon opens the narrowed section of the intestine with a lengthways cut and then reshapes it by closing it up the opposite way. Food can then pass freely through the reshaped section of the intestine. For very short strictures that are accessible by colonoscopy, it may be possible to have endoscopic balloon dilation. In this procedure, an endoscope with a balloon attached is used to widen the narrowed part of the intestine.
- Resection – if the stricture is long, or there are several strictures close together, a resection may be preferable to a strictureplasty. In a resection the surgeon removes the damaged part of the gut, and then joins together the ends of the remaining healthy sections. This join is called an anastomosis.
- Colectomy with ileostomy – for those with severe Crohn’s Disease and Ulcerative Colitis in the large intestine or colon, it may sometimes be necessary to remove most or all of the colon (a colectomy). The surgeon then brings the end of the small intestine out through an opening in the wall of the abdomen. This is an ileostomy or stoma. A bag is fitted onto the opening to collect waste.
- Stomas – click here to find out more
